One-Step Malaria Pf/Pv Ag Rapid Test,WB
- FOB Price:Get Latest Price >
- Min.Order:100 Piece(s)
- Production Capacity:Malaria
- Payment Terms:T/T , PayPal , EXW
- Favorite
Business Type:Manufacturer
Country/Region:China
Ddu Verified
HOT Rank


Span Biotech Ltd.
We are professional supplier of Rapid Tests,Elisa Kits,IVD,Diagnostical Reagents,Raw Material.
Business Type:Manufacturer
Country/Region:China
Ddu Verified
HOT Rank

INTENDED USE
The Malaria Rapid Test is a lateral flow chromatographic immunoassay for the simultaneous detection and differentiation of Plasmodium falciparum (Pf) antigen and P. vivax, P. ovale, or P. Malariea antigen in whole blood. This device is intended to be used as a screening test and as an aid in the diagnosis of infection with Plasmodium. Any reactive specimen with the Malaria Rapid Test must be confirmed with alternative testing method(s) and clinical findings.
SUMMARY AND EXPLANATION OF THE TEST
Malaria is a mosquito-borne, hemolytic, febrile illness that infects over 200 million people and kills more than 1 million people per year. It is caused by four species of Plasmodium: P. falciparum, P. vivax, P.ovale, and P. malariae. These plasmodia all infect and destroy human erythrocytes, producing chills, fever, anemia, and splenomegaly. P. falciparum causes more sever disease than the other plasmodial species and accounts for most malaria deaths. P. falciparum and P. vivax are the most common pathogens, however, there is considerable geographic variation in species distribution1. Traditionally, malaria is diagnosed by the demonstration of the organisms on Giemsa stained smears of peripheral blood, and the different species of plasmodium are distinguished by their appearance in infected erythrocytes1. The technique is capable of accurate and reliable diagnosis, but only when performed by skilled microscopists using defined protocols2, which presents major obstacles for the remote and poor areas of the world.
The Malaria Rapid Test is developed for solving these above obstacles. It detects the antibodies generated in serum or plasma in response to the infection of plasmodium. Utilizing the Pf. specific antigen (HRP-II) and pan-malaria antigen (aldolase), the test enables simultaneous detection and differentiation of the infection of P.falciparum and or P. vivax, ovale, and malariae3-5, by untrained or minimally skilled personnel, without laboratory equipment.
PRINCIPLE
The Malaria Rapid Test is a lateral flow chromatographic immunoassay. The test cassette consists of: 1) a burgundy colored conjugate pad containing mouse anti-pHRP-II antibody conjugated with colloid gold (pHRP II-gold conjugates) and mouse anti-pLDH antibody conjugated with colloid gold (pLDH-gold conjugates), 2) a nitrocellulose membrane strip containing two test bands (T1 and T2 bands) and a control band (C band). The T1 band is pre-coated with monoclonal anti-pLDH antibody by which the infection with any of the four species of plasmodia can be detected, the T2 band is pre-coated with polyclonal anti-pHRP-II antibodies for the detection of Pf infection, and the C band is coated with goat, anti-mouse IgG.
During the assay, an adequate volume of the blood specimen is dispensed into the sample well (S) of the test cassette, a lysis buffer is added to the buffer well (B). The buffer contains a detergent that lyses the red blood cells and releases various plasmodium antigens, which migrate by capillary action across the strip held in the cassette.
pHRP-II if presents in the specimen will bind to the pHRP II-gold conjugates. The immunocomplex is then captured on the membrane by the pre-coated anti-pHRP-II antibodies, forming a burgundy colored T2 band, indicating a Pf positive test result.
pLDH if presents in the specimen will bind to the pLDH gold conjugates. The immunocomplex is then captured on the membrane by the pre-coated anti pLDH antibody, forming a burgundy colored T1 band, indicating a plasmodium positive test result. In the absence of T2 band, a positive test result for any of the other three plasmodia can be recommended.
Absence of any T bands(T1 and T2) suggests a negative result. The test contains an internal control (C band) which should exhibit a burgundy colored band of the immunocomplex of goat anti-mouse IgG/mouse IgG (pHRP-II and pLDH-gold conjugates) regardless of the color development on any of the T bands. Otherwise, the test result is invalid and the specimen must be retested with another device.
STORAGE
Store the test kits at room temperature 4- 30 degrees C. The sealed pouch has a self life of 24 months.of transmitting disease.
WARNING AND PRECAUTIONS
1.For in-vitro diagnostic use only
2.All patient samples should be treated as if capable of transmitting disease.
3.Do not interchange reagents from different lots. Do not use it beyond expiration date.
REAGENTS AND MATERIALS PROVIDED
1.One pouch sealed with desiccant
2..Blood diluent buffer in a dropper bottle
3.One package insert.
MATERIALS REQUIRED BUT NOT PROVIDED
1. Clock or Timer
2. Lancing device for whole blood test
SAMPLE COLLECTION AND PREPARATION
Whole Blood
Drops of whole blood can be obtained by either finger tip puncture or veinpuncture. Do not use any hemolized blood for testing.
Whole blood specimens should be stored in refrigeration (2°Ċ-8 °Ċ) if not tested immediately. The specimens must be tested within 24 hours of collection.
Test specimens as soon as possible after collecting. Store specimens at 2 to 8 °Ċ if not testedimmediately.
Store specimens at 2 to 8 °Ċ up to 5 days. The specimens should be frozen at -20 °Ċ for longer storage.
Avoid multiple freeze-thaw cycles. Prior to testing, bring frozen specimens to room temperature slowly and mix gently. Specimens containing visible particulate matter should beclarified by centrifugation before testing.
ASSAY PROCEDURE
Step 1:Bring the specimen and test components to room temperature if refrigerated or frozen. Mix the specimen well prior to assay once thawed.
Step 2: When ready to test, open the pouch at the notch and remove device. Place the test device on a clean, flat surface.
Step 3: Be sure to label the device with specimen’s ID number.
Step 4: Apply 5ul whole blood into the sample well.Then add 4 drops of Sample Diluent. After 5min, add 2 drops again.
Step 5: Set up the timer.
Step 6: Results can be read in 30 minutes. Positive results can be visible in as short as 1 minute.
Note: Don’t read result after 30 minutes. To avoid confusion, discard the test device after interpreting the result.
INTERPRETATION OF RESULTS
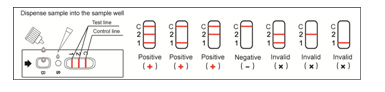
Negative: If only the C band is present, the absence of any burgundy color in the both T bands (T1 and T2) indicates that no plasmodium antigens are detected. The result is negative.
Positive:
Pf positive: In addition to the presence of C band, if only T2 band is developed, the test indicates for the presence of pHRP-II antigen. The result is Pf positive.
Pv positive: In addition to the presence of C band, if only T1 band is developed, the test indicates for the presence of pLDH antigen. The result is either Pv, Pm, or Po positive.
Mixed positive: In addition to the presence of C band, both T1 and T2 bands are developed, the test indicates for the presence of both pHRP-II and pLDH. The result is positive.
Note: Samples with positive results should be confirmed with alternative testing method(s) and clinical findings before a positive determination is made.
Invalid: If no C band is developed, the assay is invalid regardless of any burgundy color in the T bands as indicated below. Repeat the assay with a new device.
LIMITATION
1. The Assay Procedure and the Test Result Interpretation must be followed closely when testing the presence of plasmodium protozoa antigen in whole blood from individual subjects. Failure to follow the procedure may give inaccurate results.
2. The Malaria Rapid Test is limited to the qualitative detection of plasmodium protozoa antigen in whole blood. The intensity of the test band does not have linear correlation with the antigen titer in the specimen.
3. In the case of co-infection with Pf and any of the other three plasmodia, both T1 and T2 band will be developed. Thus, interpret the result cautiously when both T1 and T2 bands are visible.
4. A negative result for an individual subject indicates absence of detectable plasmodium protozoa antigen. However, a negative test result does not preclude the possibility of exposure to or infection with plasmodium protozoa.
5. A negative result can occur if the quantity of the plasmodium protozoa antigen present in the specimen is below the detection in which a sample is collected.
6. Some specimens containing unusually high titer of heterophile antibodies or rheumatoid factor may affect expected results.
7. The results obtained with this test should only be interpreted in conjunction with other diagnostic procedures and clinical findings.